Abstract
Introduction Treatment of pediatric acute myeloid leukemia (AML) requires multiple, consecutive cycles of intense chemotherapy with prolonged neutropenia and high risk for infectious complications. This treatment may have unique implications for patient health-related quality of life (HRQOL)-how patients perceive their disease impacting overall health and well-being. Patients and their families also experience significant economic burdens associated with disease and treatment. In particular, patients from socioeconomically vulnerable families disproportionately experience economic burden, which may subsequently worsen HRQOL. Few studies have explored the influence of household income (HHI) on HRQOL during AML therapy. Furthermore, the mechanisms through which HHI may influence HRQOL have not been described. To fill this gap, we examined the association between HHI and HRQOL and explored whether differences in presentation acuity or treatment toxicity mediate this association.
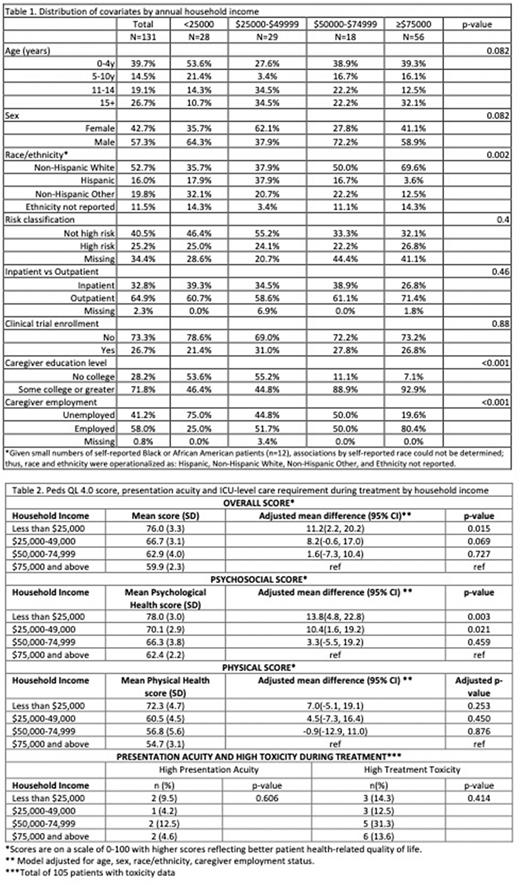
Methods Secondary analyses were performed using data from a multi-institution, prospective cohort study in pediatric patients receiving treatment for newly diagnosed AML. Patients and their primary caregivers were recruited to complete prospective assessments of patient HRQOL, and a detailed survey providing sociodemographic information including annual HHI (<$25K; $25K-49K; $50K-74K; and >$75K). HRQOL was measured using caregiver proxy responses to the PedsQL 4.0 Generic Core Scales; overall score and separate scores for the psychosocial and physical health subscales were evaluated. Daily-level inpatient resource utilization (RU) data were obtained via a merge with the Pediatric Health Information System database. High acuity at initial presentation was defined as any ICU-level RU within the first 72 hours following first leukemia admission. High treatment toxicity was defined as any ICU-level RU requirement during treatment. Covariates including patient age at diagnosis, sex, race/ethnicity, risk classification, clinical trial enrollment, and inpatient vs outpatient neutropenia management were obtained from electronic medical record abstraction. Linear regression models compared HRQOL by categories of HHI (reference: HHI >$75K). Demographic and clinical characteristics were compared for patients who enrolled on the study and those who were eligible but were not enrolled to evaluate for potential selection bias.
Results 225 eligible patients were identified from 14 institutions, and 60% of eligible patients enrolled on the study. Patients with lower HHI were generally younger, more likely to be non-White, their caregivers were less likely to be college educated and more likely to be unemployed compared to those with higher HHI (Table 1). Overall HRQOL scores were low (mean ±sd: 65.7 ±1.8). Patients in the lowest HHI category had higher (better) overall HRQOL as compared with patients in the highest HHI category (mean ± sd: 76.0 ±3.3 for HHI <$25K vs. 59.9 ±2.3 for HHI>$75K, adjusted mean difference: 11.2, 95% CI: 2.2-20.2). Subscale assessments revealed larger differences on the psychosocial domain than physical domain (Table 2). Overall, 6% of patients presented with high acuity and 16% had high toxicity; there were no clear trends in presentation acuity or toxicity by HHI (Table 2). HRQOL scores were comparable for patients with (62.0 ±19.5) and without high toxicity (66.2 ±18.2). Enrolled patients were less likely to be Black or African American (9.6% vs 20%), more likely to be privately insured (51.1% vs 42.2%), and more likely to have been treated on a clinical trial (27.4% vs 17.8%) than eligible patients who did not enroll on the study.
Conclusion Patient HRQOL during AML therapy is low overall. Contrary to our hypothesis, lower HHI was associated with superior HRQOL, particularly in the psychosocial health domain. HRQOL did not differ by toxicity, and toxicity did not differ meaningfully by HHI, refuting a mediating role in this association. These findings could potentially indicate differences in perspective on HRQOL amidst cancer therapy. Future studies to qualitatively investigate patient- and caregiver-reported drivers of HRQOL among low and high-income cohorts are warranted. Given the observed differences in characteristics for enrolled versus unenrolled patients, we cannot rule out a potential selection bias. Formal quantitative bias adjustment is ongoing.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal